Workers compensation claims typically take longer to process compared to commercial insurance claims. It is crucial that your staff submit clean work comp claims with proper documentation in a timely manner. In this article we will discuss the top reasons for work comp denials and how to stop them.
1. No Time Spent in Documentation
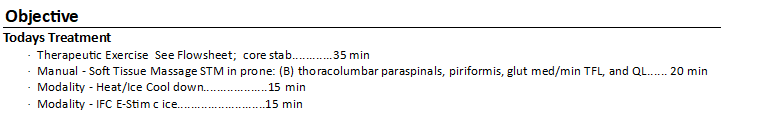
Recently, our billing staff has begun to see an increase in denials for work comp claims when providers do not document the time spent for each billed code. More work comp insurance companies now require that the treatment time spent be included in the providers documentation. Failure to include these notes can lead to denials and delay reimbursement. While this is not a mandatory rule, it is recommended that your therapists add time spent for each code to eliminate these denials. Check out the image below for an example of how notes will look for your therapists:
2. Treatment Not Related to Work Injury
When an injured patient is receiving physical therapy for their active workers compensation case, treatment should be specific to the injury preventing them from returning to work. For example, if a patient injured their knee on a job site and is ordered to attend physical therapy, they should not receive physical therapy for their shoulder.
Insurance adjusters will deny claims if treatment is not related to the work injury. We recommend scheduling separate appointments to address separate injuries and billing the patient’s private insurance or have the patient agree to a self-pay rate for any non-work-related injuries. Doing this will ensure that the claims submitted under the work comp case are not denied.
3. No Independent Medical Examination (IME)
Certain patients involved in work comp cases are required to have an examination with a doctor selected by the insurance company, known as an independent medical examination (IME). The doctor will assess the extent of the patient’s injury and the progress of recovery to determine if the recommended treatment is justified. If the patient does not attend their IME, the insurance company may terminate their medical coverage, resulting in denied claims. If the billing department receives a denial for “Failure to Attend IME”, we recommend postponing treatment until the patient’s attorney and/or work comp adjuster rectify the situation.
Denied work comp claims can quickly cause congestion in your accounts receivable. Practice owners and managers who implement our recommendations will see quicker turnaround for reimbursement and decrease the chance of write-offs. Are Claim Denials negatively impacting your practice? A billing assessment by industry experts can identify areas that need improvement and offer solutions. Learn more here.