Credentialing has never been synonymous with fast. Many healthcare providers get frustrated with the long wait times (90-120 days) associated...
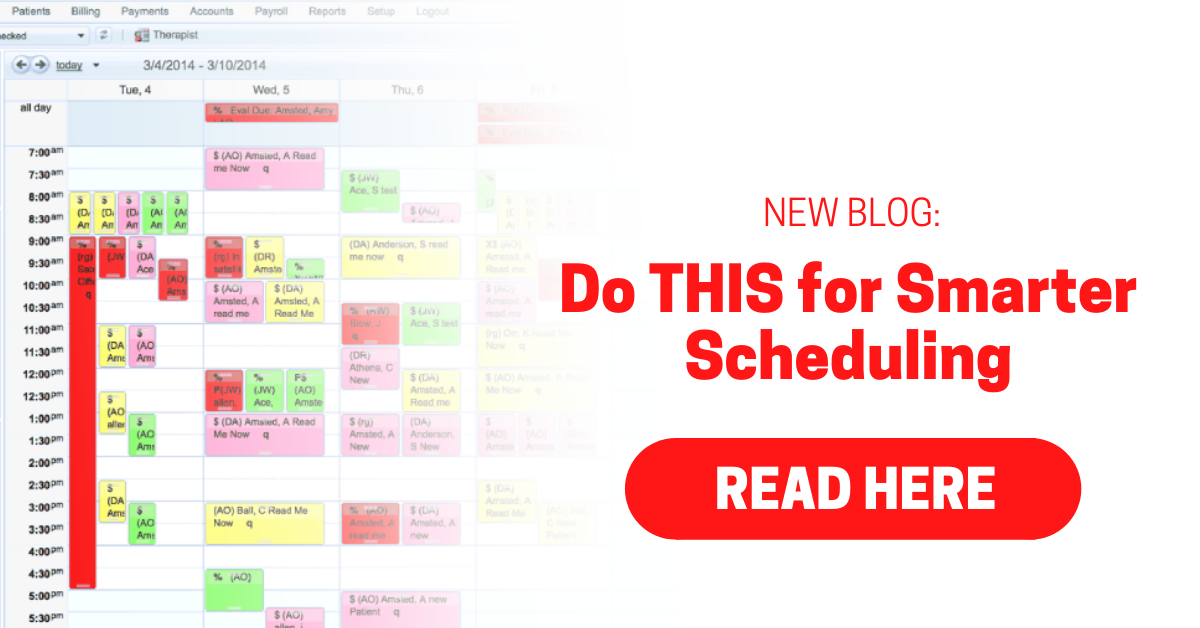
Creating an exceptional experience for your patients involves convenient and efficient scheduling. Having a fine-tuned scheduling process will...
The front desk can be hectic with patients coming in and out, phones ringing, and time-sensitive tasks needed to be done. Your front desk staff is...
Setting goals for your employees is a great way to keep them engaged while improving the productivity of your practice. Check our recommendations...
Billing Credentialing Management
1. PTA/OTA Reimbursement Cut Takes Effect in 2022 It’s been a year since CMS implemented CO/CQ modifiers for services provided “in whole or in part”...
Is your staff struggling to get their tasks done every day? Whether it’s because they can’t do the work or they won’t do the work, productivity is...
What is an insurance referral?
Chatty Front Desk Has Frightening Consequences A physical therapy practice in North Carolina failed to address issues at the front desk, leading to a...
There are two types of write-offs in medical billing: necessary and unnecessary. Necessary write-offs include contractual obligations, small balance...






.png)